
Introducing Team 1 of the Green Surgery Challenge
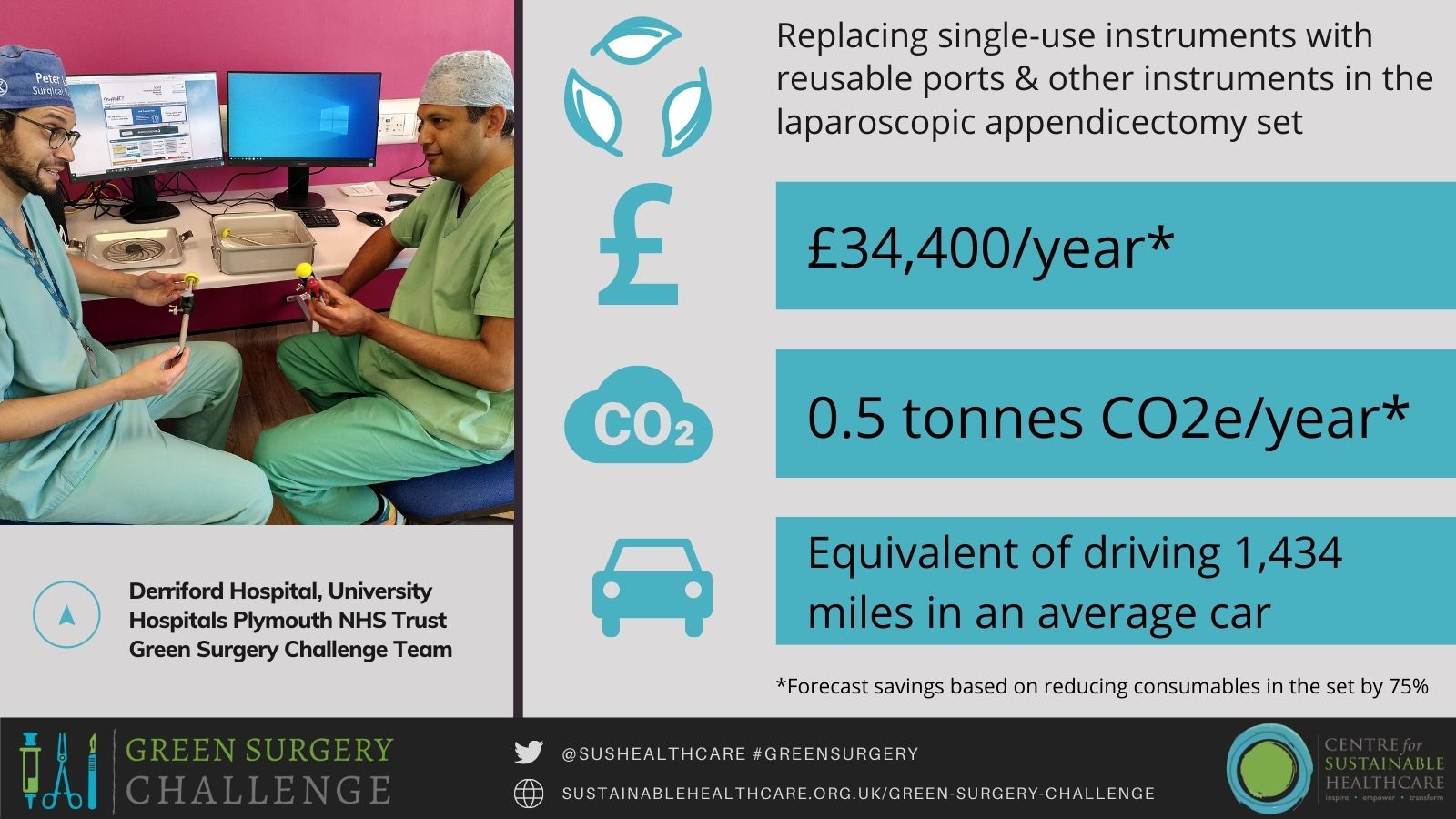
The team at Derriford Hospital, University Hospitals Plymouth NHS Trust, focused on reducing the consumption of single-use surgical equipment for their Green Surgery Challenge project. Consumables account for one-third of surgical procedure-related emissions and so a reduction has the potential to make a significant impact on carbon emissions in their department and Trust.
The team was led by Mr Peter Labib, ST6 general surgery registrar and Dr Bryony Ford, Foundation Year 2 doctor; Ms Michelle Winfield, Senior Sister & Clinical Procurement Specialist who was pivotal to the success of the project, liaising with company representatives and the Sterilisation & Decontamination Unit; the project leads were supported by Mr Aditya Kanwar, Consultant Hepatobiliary Surgeon, Mr Grant Sanders, Consultant Oesophagogastric Surgeon, and Mr Walter Douie, Consultant Colorectal Surgeon.
Read the full case study here.
Summary
The team carried out their project using the Sustainable Quality Improvement (SusQI) framework. First, they introduced their colleagues to the concepts of sustainable healthcare; how the climate crisis has health impacts, and how surgery is contributing to the climate crisis. Following this well-received presentation, the team surveyed their colleagues to find out about surgical practice in their department so that they could identify the hotspots of consumption of single-use surgical instruments.
In the survey, many colleagues reported frequently opening disposable instruments during laparoscopic appendicectomies, which is one of the most frequently performed procedures in their department (each year, around 500 appendicectomies are performed at Derriford Trust) and nationwide. Surgeons’ reasons for not using the existing ports were also surveyed. The team then carried out an audit that showed that single-use ports and Johann graspers were opened in every case; single-use scissors and Marylands were opened occasionally.
Ms Wingfield and Mr Labib researched, costed, and procured reusable instruments (including ports with specifications that would address the surgeons’ concerns). Mr Labib and Dr Ford then meticulously modelled the environmental and financial impacts of the change, using carbon footprinting methodology and procurement prices. The team was then able to propose a revised laparoscopic appendicectomy procedure set that included reusable replacements for the single-use items that are commonly used. They found that the proposed updated appendicectomy set would significantly reduce both the carbon footprint and the financial cost of laparoscopic appendicectomies.
The appendicectomy set will be changed once formal feedback on the new reusable ports is completed (informal feedback has been positive) and the team will repeat the audit to demonstrate if the changes have successfully reduced consumable use. The social impact will be assessed by surveying the surgical team’s satisfaction with the replacement set.
In addition to the changes they have made, the team have become influencers and catalysed significant cultural change in their department, division, and in the Trust. Their colleagues have been inspired by the team's Green Surgery Challenge project to work on changing other surgical sets, there is discussion in the surgical department about switching off air conditioning in elective theatres overnight (this would have the forecast impact of reducing energy usage by up to one third, which alone could allow the department to meet their target of a 20% reduction by 2025 target given the contribution of energy to the overall emissions from theatres), the team is presenting their project to the Trust Board, and one team member has been invited to join the new University Hospitals Plymouth Sustainability Committee.
Carbon and Financial Impact
The project has forecast annual savings of £34,400 and 0.5 tonnes CO2e/year (based on reducing consumables in the set by 75%). This is the same amount of CO2e as driving 1,434 miles* in an average car (2.5 times from G7 to COP26).
*CO2e comparison: Distance from G7 (Carbis Bay, Cornwall) to COP26 (Glasgow): 573 miles / 922 km. Average car (unknown fuel) GHG emissions: 0.34851kgCO2e/mile.
Dr Olivia Bush, Programme Lead for Sustainable Clinical Practice at the Centre for Sustainable Healthcare, said:
“This team were especially successful in engaging large numbers of their colleagues to contribute to identifying the hotspots of single-use surgical instruments in their department and to implement this project. This broad engagement has paid off as we’ve seen by the significant and impressive ripple effects of the project on changing the culture within their department and University Hospitals Plymouth NHS Trust as a whole.”
The Green Surgery Challenge is a special adaptation for clinical specialties of the Centre for Sustainable Healthcare’s flagship programme, the Green Ward Competition (an award-winning clinical leadership and engagement programme to improve the environmental sustainability of healthcare). The challenge has been created and delivered through collaboration with a group of supportive partners including NIHR MedTech Co-operative in Surgical Technologies, Royal College of Surgeons England, Royal College of Surgeons Edinburgh, The Sustainable Healthcare Coalition, Brighton and Sussex Medical School and the Association for Perioperative Practice. The Challenge has been made possible through the generosity of our Gold Funders and Sponsors NIHR MedTech Co-operative in Surgical Technologies and Elemental Healthcare, Silver Sponsors Royal College of Surgeons England and Royal College of Surgeons Edinburgh, Bronze Sponsors the AHSN Network, Vanguard Medical Remanufacturing, and Bowa Medical UK. For more information, please click here.

